Functional Medicine: A Primer
Is this the future of medicine or just another overblown medical fad?

In my clinic it seems as if everyone is looking for a more holistic approach to health. There is a patient-led demand for a change in medical care. What is more, every week there appears to be a new scientific discovery that could radically reshape the practice of medicine. And yet, the actual delivery of health care has changed little over the last decade.
This is mind boggling to me—especially as my own practice has changed drastically in the same timeframe:
- From a standard family medicine practice…
- Then, to start a pharmaceutical clinical research group, incorporate integrative medical testing and metabolic evaluations with my patients,
- And finally, to starting a new practice in Functional Medicine.
It seems to me that the field of medicine should have had a similar trajectory and change rate, yet there have been no major breakthroughs in the delivery of health and application of medical advances.
Yet at places like The Cleveland Clinic’s Functional Medicine Clinic and the University of Arizona’s Integrative Medicine Center, a new way of delivering health has been developed that is changing the landscape of how we view health and disease and the health care delivery model. This new specialty of medicine is referred to as either Integrative Medicine or Functional Medicine. In this article, I will explain this new way of thinking and evaluating patients—to frame a new discussion as to how medicine should be practiced in the 21st century.
Let’s begin by examining the shortfalls of the current standard-of-care…
Example:
A Patient With Diabetes
Suppose a patient comes to my office with undiagnosed diabetes. Diabetes is a disease entity defined by either: 1) a random sugar over 200, 2) three fasting sugars over 125, or 3) a hemoglobin A1c of 6.5 or greater. Once one of these levels is reached, a diagnosis of “Diabetes” is obtained and the first line medication of metformin is prescribed with recommended diet and lifestyle changes. If adequate control is not reached, then second line medications are prescribed (e.g. Januvia, Onglyza, Invokana, Jardiance). If these don’t result in control, further medications are prescribed, and ultimately insulin is begun.
The problem with this approach is that it jumps too quickly to a treatment without adequately understanding the root cause of my patient’s diabetes. Yes, she has elevated sugar levels caused by insulin resistance, but what caused the insulin resistance? Is her current insulin resistance the result of years of sugar and carbohydrate consumption? Or, is her insulin resistance caused by food and environmental chemicals called endocrine disrupters? Underlying inflammation can contribute to insulin resistance as well as trans-fat consumption causing the cell membranes to harden and resulting in the ineffective working of any receptor (like the insulin receptor) attached to that membrane. Heavy metal exposures from arsenic (exposures include metallurgy or eating certain foods) or mercury (from silver fillings, solder in piping, consumption of high mercury seafood like tuna) are directly correlated to increased incidence of diabetes. Finally, chronic infections, like dental cavities or periodontal disease, are now known to be associated with uncontrolled diabetes and drug-resistant diabetes.
As you can see, something as basic as diabetes can quickly turn into a very complex disease process with multiple underlying causes and thus interdependent and interrelated treatment strategies. So, shouldn’t our medical practices reflect this known complexity in how we deal with patients and their chronic diseases? If research is uncovering this interconnected web of insults and disease states, shouldn’t the standard-of-care reflect this new-found knowledge? If it doesn’t, why not?
Something as basic as diabetes can quickly turn into a very complex disease process with multiple underlying causes and thus interdependent and interrelated treatment strategies.
Functional Medicine is a model-of-care designed specifically to move beyond merely treating symptoms. Instead, Functional Medicine seeks to understand (and therefore treat) the root cause of disease and dysfunction.
So What Is Functional Medicine?
A Definition:
Functional Medicine is a unified & holistic, patient-centered methodology of delivering medical care with the goal of maximizing the individual’s wellness.
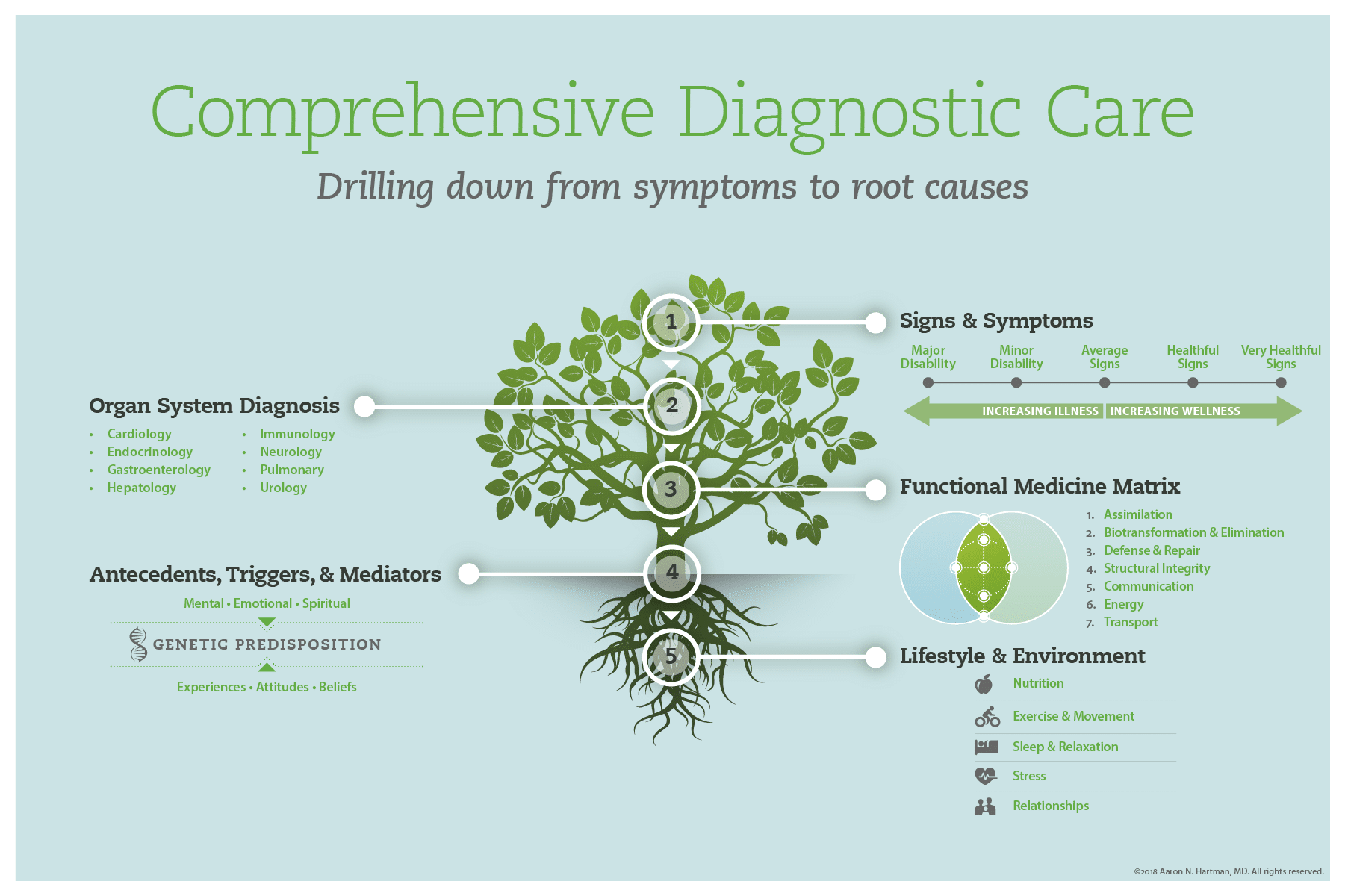
This methodology progressively examines:
- Signs & Symptoms
- Organ System Diagnosis
- The Functional Medicine Matrix
- Antecedents, Triggers, & Mediators
- Lifestyle & Environmental Factors
The Functional Medicine Matrix
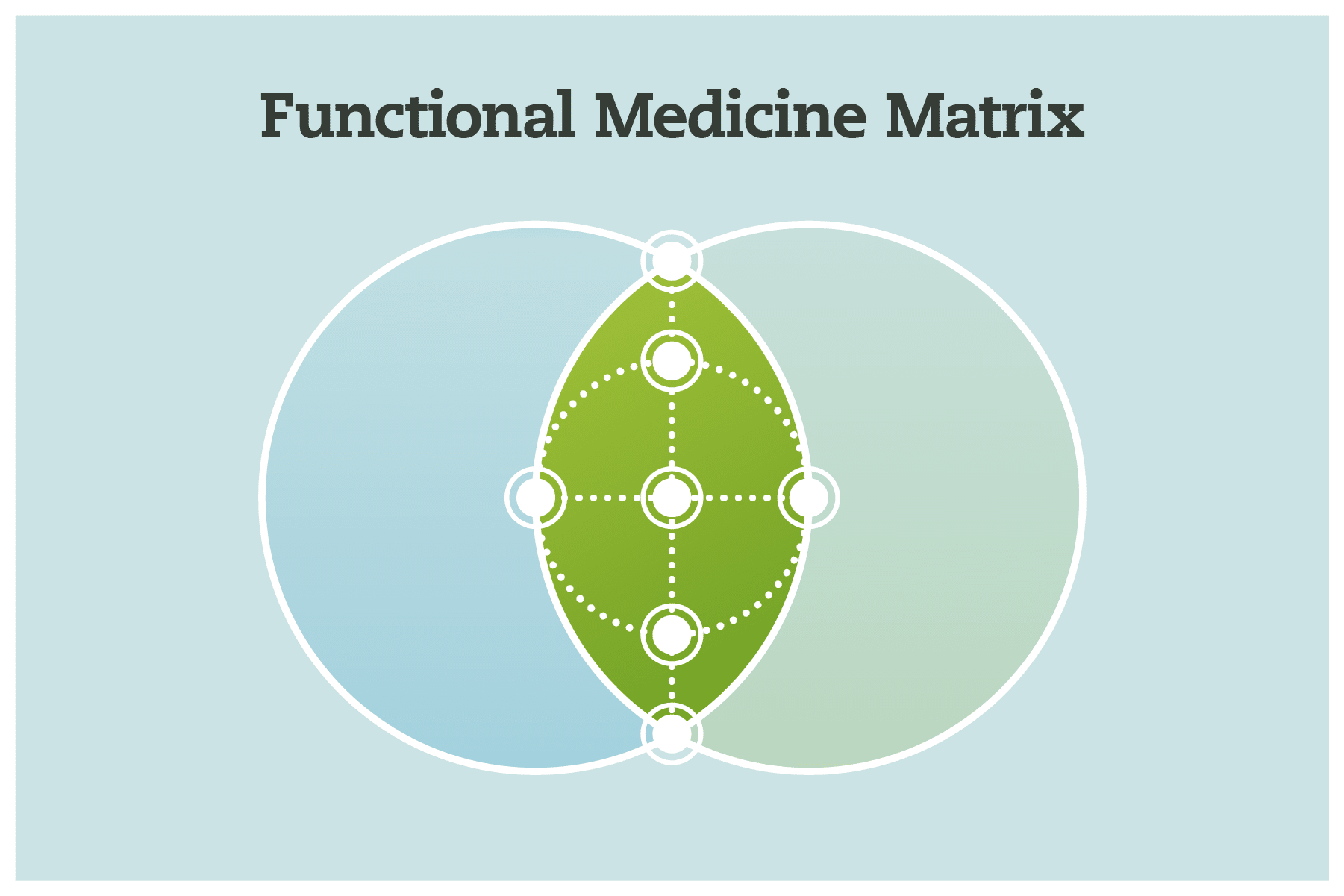
In addition to providing a more comprehensive philosophy of care, Functional Medicine introduces a focus on interconnected biologic systems in contrast to independent organ systems—looking at the interplay of physiology and function.
Functional Medicine focuses on seven interconnected biologic systems called the Functional Medicine Matrix.
- Assimilation: Digestion, absorption, microbiota, respiration
- Defense and Repair: Immune system, inflammation, infections/microbiome
- Biotransformation & Elimination: Toxicity & detoxification
- Energy: Energy regulation/production, mitochondrial function
- Transport: Cardiovascular and lymphatic systems
- Communication: Endocrine system, neurotransmitters, immune messengers
- Structural Integrity: From musculoskeletal system to subcellular membranes
As an example of how these systems work together (and contribute to dysfunction), someone diagnosed with Chronic Fatigue Syndrome may not only have chronic fatigue—loss of energy and decreased exercise tolerance (Energy)—but also abnormal hormone levels and sleep/wake cycles (Communication) as well as digestive issues/gas/bloating (Assimilation) and recurrent injuries (Structural Integrity). Their brain fog, lack of ability to concentrate and quick mental fatigability (Energy + Communication) limits their ability to handle their every day life.
From a Functional Medicine approach I would attempt to see how all these systems are interrelated and in what order they became dysregulated. Only then can we attempt to ‘unwind’ these tangled systems.
Antecedents, Triggers, & Mediators
In this model I also take into account the patient’s medical history viewed through the lens of ATMs (Antecedents, Triggers & Mediators).
Antecedents
What preceded the development of my patient’s thyroid disease leading up to her diagnosis?
This could be poor diet, lifestyle, birth history, or even environmental factors.
Triggers
Then, I attempt to discover the triggers that pushed her over the edge into autoimmunity. Was it an acute infection, one last bout of bronchitis/pneumonia, or even the car accident resulting in a concussion?
Mediators
Finally, what event(s) are keeping the fire going? This could be poor sleep, chronic stress, work environment or even current/ongoing mold/lyme exposure.
As you can see in this model, the complexity continues to develop as we weave web upon web to help uncover the root cause of an individual’s current health condition.
Lifestyle & Environment
After uncovering the antecedents, triggers, & mediators resulting in the current dysfunction—a combination of lifestyle & environmental factors interacting with a patient’s specific genetic predispositions—I work with my patient to progressively unwind those specific lifestyle & environmental factors.
This approach is sometimes called Lifestyle Medicine due to the emphasis on diet, nutrition, sleep, exercise, stress, and relationships. While these are all included and addressed in the Functional Medicine model, this model is more comprehensive than merely recommending lifestyle interventions.
Conclusion
Functional Medicine is a radically new way of looking at someone’s state of health—integrating their entire history and symptoms into a cohesive way of dealing with their health. It includes a patient’s symptoms but also incorporates our understanding of specialty/organ system care, and doesn’t stop there. It divides these into the Functional Medicine Matrix for evaluation, incorporates the patient history, and then synthesizes these with her lifestyle and environment. This is true Personalized Medicine! Based on the patient’s needs and preferences but structured around his entire health history and medical presentation.
As you can imagine, this kind of evaluation is time consuming. On average, it takes me two hours to perform the initial evaluation, another 45-60 minutes to review the corresponding labs, then another 45 minute follow-up with the patient to review the labs and formulate a starting treatment plan. And this is just the beginning of a patient’s evaluation.
If you’d like to learn more about Functional Medicine, take a look at my reading list. As I read more books that I feel will be of use to people, I will routinely update this page.
Below is a real-life example of someone I am caring for with the diagnosis of Inflammatory Bowel Disease. As you read it, notice how everything weaves together. Notice not only how my treatment plan changes based on advanced diagnostic testing and the patient’s response, but how comprehensive the treatment is—how every aspect of the patient’s history is woven into the care plan. In the Functional Medicine model, each patient receives an individualized care plan just like this.
So, is this the future of medicine, or just another passing fad?
Case Study:
Inflammatory Bowel Disease
After uncovering the antecedents, triggers, & mediators resulting in the current dysfunction—a combination of lifestyle & environmental factors interacting with a patient’s specific genetic predispositions—I work with my patient to progressively unwind those specific lifestyle & environmental factors.
This approach is sometimes called Lifestyle Medicine due to the emphasis on diet, nutrition, sleep, exercise, stress, and relationships. While these are all included and addressed in the Functional Medicine model, this model is more comprehensive than merely recommending lifestyle interventions.