Chronic Health Issues
Chronic Health Issues Are On the Rise
Addressing the Seismic Shift from Acute to Chronic Healthcare

Dr. Aaron Hartman
December 5, 2023

Chronic Health Issues Are On the Rise
The prevalence of chronic health conditions is rising at an alarming rate.
Over the last 10 – 15 years, medical professionals have begun to distinguish between acute-care issues (e.g. heart attacks, strokes, and trauma) and chronic health issues like recurrent heart disease, neurological conditions, autoimmune diseases, cancer, chronic fatigue, depression, anxiety, and other brain-inflammation health problems.
Chronic health issues are now the most common problems we deal with.
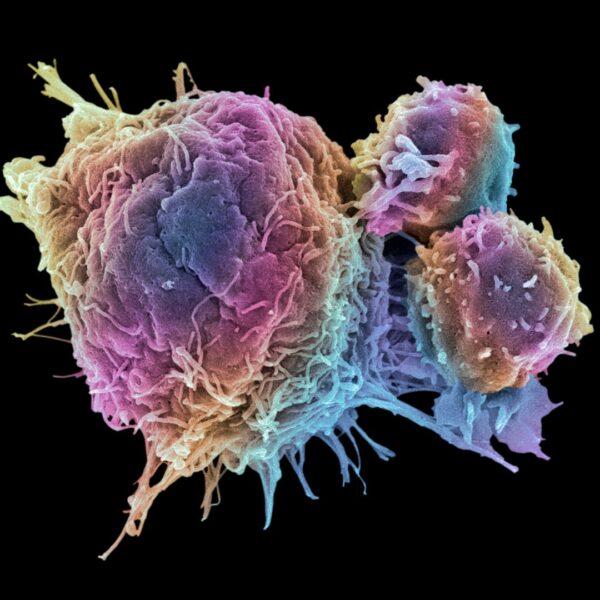
Chronic health issues are now the most common problems we deal with. For example, half of us will die of some kind of heart disease. Neurological conditions are becoming quite common, even in the very young. One out of 12 people has some form of autoimmune disease, like Hashimoto’s, hypothyroidism, rheumatoid arthritis, or multiple sclerosis, while about 20% of Americans have a positive autoantibody. Currently, one out of every two Americans is expected to get some kind of cancer in their lifetime. Neurological conditions used to be rare, but are now quite common and include Alzheimer’s disease, autism, PANDAS, ADHD, and many more.
Many of my colleagues who have been practicing functional medicine for 30 – 40 years have noted changes in functional medicine over time. Several decades prior, patients suffering from chronic issues needed only basic changes to improve their health. Now, it seems that with inflammation and nutritional deficiencies, patients are getting sicker and require more complicated, individualized care.
How You Can Avoid the Wave of Chronic Health Issues?
In this article, I’d like to address this (entirely appropriate) medical shift from acute-care to chronic health issues. I hope to shed light on common causes for our increasing health issues. I will also highlight how basic lifestyle factors like diet, exercise, and sleep, as well as addressing environmental conditions can not only improve your overall wellness but also help prevent some of these debilitating chronic health issues.
Let’s start by untangling some admittedly confusing chronic health issues: autoimmune and autoinflammatory diseases.
Autoinflammatory & Autoimmune Diseases
Both autoinflammatory and autoimmune diseases involve your immune system (though different parts), and both result from cellular inflammation. There is a lot of overlap in language and final effect, so it’s understandable if you are confused. Let’s try to clear up that confusion.
Autoinflammatory and autoimmune diseases arise from two different aspects of your immune system, producing distinct but overlapping effects.
| Autoinflammatory | Autoimmune |
|---|---|
| Hyperactivation of the innate immune system. | Dysregulation of the adaptive immune system. |
| Dysregulated cytokine production | Production of autoantibodies |
Disease Examples:
|
Disease Examples:
|
Your Awesome Immune System
Did you know the average person has 10 active viruses in their body at any point in time? This is normal!
Even when you brush your teeth, you can get ecoli and other bacteria from your mouth into your bloodstream for a short period of time. The immune system is so effective that your spleen can filter these things out. Your liver can filter out substances from the GI tract. And even though you have these transient bacteria, yeast, and fungi in your blood, they don’t cause disease.
Our bodies are designed to handle these substances without over-reacting!
In order to properly understand autoimmune and autoinflammatory diseases and treat chronic health issues, we have to understand how to support our immune system so it can take these normal, day-to-day stimuli in stride.
Autoinflammatory Diseases
Hyperactivation of the innate immune system resulting in dysregulated cytokine production
Your innate immune system is the part of your immune system you were born with. It’s non-specific, has been pre-programmed to act a certain way, and does not adapt. While your adaptive immune system can take 10 – 14 days to produce antibodies, your innate immune system stands ready to respond very quickly (within seconds) to kill viruses, cancer cells, and other foreign invaders that your body is exposed to.
Problems arise when it’s been overactive for a long period of time and gets stuck in the wrong position. An autoinflammatory disease can be the result.
Dysfunctions of the Innate Immune System
Some of the diseases that fall into this category include things like Mast Cell Activation Syndrome (MCAS), small intestinal bacterial overgrowth (SIBO), Autoimmune Inflammatory Syndrome Induced by Adjuvants (ASIA syndrome), as well as different adjuvant-based illnesses like post-infectious illnesses. These can include post-Lyme, post-mono, or Long-COVID. In these cases, people contract an acute viral infection and then experience lingering inflammation after they’ve cleared the virus.
Mast Cell Activation Syndrome (MCAS)
Mast cells are cells that release histamine in your body. Typically the innate immune system attacks and destroys viruses, particulates, toxins, etc, and then activates mast cells which release inflammatory mediators.
Small Intestinal Bacterial Overgrowth (SIBO)
SIBO is an imbalance of gut bacteria in the GI tract and can result in IBS or other gastrointestinal problem including excessive gas, bloating, GI discomfort, food sensitivities, etc. SIBO also falls into the category of these autoinflammatory diseases because the low-grade bacteria in the small intestine, where it shouldn’t be, can activate mast cells. So SIBO can sometimes look like MCAS and sometimes look like CIRS, another autoinflammatory condition.
Adjuvants-Based & Post-Infectious Illnesses
Dr. Yehuda Shoenfeld, one of the top immunologists in the world, wrote the textbook on vaccines and immunity and he also identified Autoimmune Inflammatory Syndrome Induced by Adjuvants (ASIA Syndrome).
In his research, he found four major causes of autoinflammation:
- Silicone (as from silicone implants)
- Adjuvants (like aluminum or petroleum products)
- Chronic Infections
- Leaky Gut
Pay special attention to those last two. I’ll return to them.
But let’s move on to the other category of dysfunction within our (adaptive) immune system.

Autoimmune Diseases
Dysregulation of the adaptive immune system resulting in the production of autoantibodies
 |
 |
 |
On the Rise…
When I was in medical school in 1996, I was told that I would not see autoimmune disease in practice. I was taught that autoimmune diseases were rare and that treatment would be limited to the realm of specialists and universities. Diseases like celiac disease, rheumatoid arthritis, and even PANDAS were conditions I would never see. We discussed autoimmune diseases only for academic purposes because, supposedly, I would never need to treat them.
My how times have changed! Currently, 1 out of 12 people have some kind of autoimmune disease and 1 out of 5 has a positive autoantibody. Autoimmune diseases are the second or third most common cause of chronic illness in the country.
What Are Autoimmune Diseases?
Ideally, our immune system is designed to do nothing 99.999% of the time. It’s supposed to see bacteria in your gut, viruses you’re exposed to, yeast in your GI tract, dust, chemicals … and ignore them. Your immune system isn’t supposed to respond to these things.
Sometimes, however, chemicals from the environment — either synthetic or natural — bind to your cells, change the shape of those cells, and start creating a little cellular inflammation. As that inflammation increases, eventually the body begins producing autoantibodies to combat this process, but attacking your own inflamed cells rather than foreign objects. Over time, that inflammation can increase to the point that autoimmune disease results.
A Trajectory Toward Autoimmune Disease
On average, a person will have a positive thyroid autoantibody for about 8 – 10 years before they’re diagnosed with Hashimoto’s hypothyroidism. Someone can have a positive automitochondrial antibody (AMA) test for 15 – 20 years before they’re diagnosed with lupus.
So we can see a spectrum of low-grade inflammation from toxins, which over time, triggers your adaptive immune system to start activating against itself.
Four preconditions are needed to develop an autoimmune disease:
- Genetic Predisposition
- A Chronic Infection
- Leaky Gut
- A Triggering Event
Chronic Infections can come from things like mono, viral infections like herpes simplex virus (HSV), chronic strep infections, and chronic GI infections. Leaky Gut is a dysregulation of your intestinal lining, allowing toxins into your bloodstream and causing an inflammatory response. Triggering Events can be almost anything: a trauma in the past, a head concussion, a severe accident with hospitalization, etc.
Note the critical role of addressing gut health and chronic infections, 2 of the 4 preconditions, which are the only two within our control. And they are 2 of the 4 causes of autoinflammatory issues noted above.
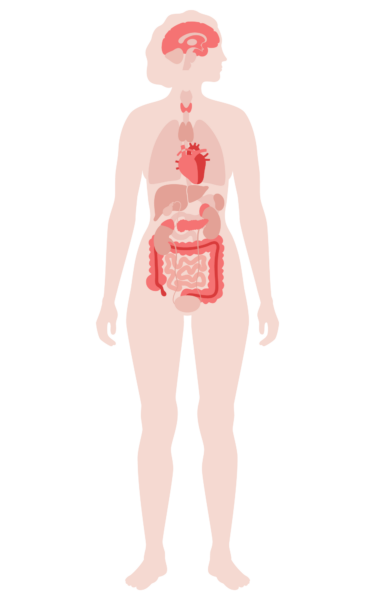
Autoimmune Diseases Are Systemic
The world of traditional medicine generally compartmentalizes autoimmune diseases. If you have thyroid autoimmune disease, you see a endocrinologist. If you have a joint issue like rheumatoid arthritis, you see a rheumatologist. If you have inflammatory bowel disease, you see a gastroenterologist. But we now understand that all autoimmune diseases interact with each other.
While you might mainly experience joint symptoms from rheumatoid arthritis, or thyroid symptoms from Hashimoto’s, the reality is that every autoimmune disease is systemic. For example, some people with celiac disease will present with tics, ADHD, and seizures. Some people with Hashimotos will present with fatigue, brain fog, and fertility issues. Patients with rheumatoid arthritis might present with lung issues since rheumatoid often also affects the lungs.
Now that we know that autoimmune diseases are systemic, we can see why they must be addressed holistically, treating the patient as a whole. I’ll come back to this point later.
I’ve highlighted that chronic infections and leaky gut are causes of both autoimmune and autoinflammatory diseases. Therefore, it’s probably worth diving a bit deeper into the unique role of chronic infections.

Chronic Infections
I confess that chronic infections were a puzzle to me for years. Before studying functional medicine, I’d never heard of chronic infections causing anything. And yet, I had some patients with inflammatory bowel disease who did not respond to the treatment. I had patients with Crohn’s disease, ulcerative colitis, and celiac disease that just didn’t get better, regardless of what was being done by their specialists.
As I researched chronic infections, I discovered that about 30% of kids with resistant Crohn’s disease actually have a chronic viral infection in their GI tract. I also learned how chronic yeast issues in the GI tract can be related to Crohn’s as well as other inflammatory diseases. And I discovered that Quest Laboratories had created an autoantibody test, an anti-vinculin, that can be used to diagnose Crohn’s disease.
Chronic Infections: An Underlying Cause of Disease
We’re learning that chronic infections are a big player in cardiovascular disease, neurological diseases, and gastrointestinal disorders, as well as being mandatory for autoimmune diseases.
Take, for example, mononucleosis (mono), which 80% of the population gets by the time they reach adulthood. If the body doesn’t control the infection, a low-grade, chronic Epstein-Barr virus (EBV) can lead to Hashimoto’s, multiple sclerosis, and other autoimmune diseases.
Unfortunately, chronic infections spin a wider web of dysfunction. The research of Dr. Bredesen from the Buck Institute at UCLA, notes that Type 3 Alzheimer’s includes those with spirochetes in the brain, which causes buildup of beta amyloid. Colon infections, like yersinia, as well as different kinds of ecoli can lead to inflammatory bowel disease. Other infections, both viral and bacterial can also result in dysregulation of the immune system. These include: chronic Lyme and other tick-borne illnesses; chronic viral infections like Epstein-Barr and herpes simplex virus; and bacterial overgrowth in the GI tract like small intestine bacterial overgrowth (SIBO).
It is surprising, then, that chronic infections are not often discussed as a treatment option. Perhaps the main reason chronic infections are overlooked is that there aren’t any medications on hand to treat them. Additionally, the symptoms are often opaque; sympts might include aches and pains, poor sleep, anxiety, mood swings, problems focusing, learning problems, or other very general symptoms.

Mold-Related Illnesses
Mold is another major culprit in chronic health issues. Although I’ve written extensively about mold-related illness (also referred to as Chronic Inflammatory Response Syndrome or CIRS), it’s worth highlighting its connection to chronic health issues.
You might pick up from the complex name “Chronic Inflammatory Response Syndrome” that CIRS is essentially the body responding to chronic inflammation. In this case, that chronic inflammation is the result of being exposed to a biotoxin. Mold, and the company it keaps, is the most common source and simplest shorthand for an array of biotoxins that often go undetected for an extended period, leading to chronic inflammation and then dysregulation of your immune system.
Why Awareness of Mold-Related Illnesses is So Important
First, this problem is also on the rise. As we build our homes and offices to be more energy-efficient, the unintended consequence is reduced airflow. We now have more recirculated air with higher levels of volatile organic compounds (VOCs). Mold, and the “friends” that it keeps such as endotoxins, VOCs, actinomyces, particulates, and other bacteria particles, are just a few of the 40+ unhealthy substances we know about that occur in water-damaged buildings (WDBs). We’ve created houses that are more energy-efficient but also more toxic.
We’ve created houses that are more energy-efficient but also more toxic.
Second, even if you aren’t suffering from full-blow CIRS, you may still be struggling with chronic health issues relate to mold. Mold and other related toxins can cause varying levels of inflammation. Many people experience basic allergic reactions to mold without realizing it. For example, 23% of all asthma is related to indoor mold. Toxin exposure can also cause systemic inflammation. As a result, some people experience fertility issues, gut issues, and small intestine bacterial overgrowth (SIBO). CIRS is an extreme version of these reactions, but many people exposed to mold suffer from less extreme, yet very problematic, responses such as low-grade inflammation, fatigue, brain fog, and memory issues.
23% of all asthma is related to indoor mold.
These toxicity-related problems have become one of the major causes of illness we routinely see in our clinic and work with our patients to help them get better.
Solutions & Support
A Functional Medicine Approach to Chronic Health Issues
If all of this still feels confusing, that’s understandable because so many of these conditions overlap. About 80% of MCAS sounds like SIBO, and 80% of SIBO sounds like ASIA syndrome. ASIA syndrome sounds a lot like CIRS. There is a lot of crossover between these different conditions.
To truly help people with chronic health problems, it’s not enough to be an expert in chronic Lyme disease or post-Lyme syndrome. You also need to know about mold toxicity and CIRS. You can’t just know about CIRS, you have to understand SIBO as well as ASIA syndrome, hypermobility, and MCAS. Especially as we witness advancing chronic health issues with multiple layers, we need functional medicine practitioners who can individualize healthcare and take a whole-person approach.
This is where functional medicine shines. Functional medicine addresses the whole immune system (innate & adaptive) by focusing on gut health, sleep, stress reduction, nutritional deficiencies, environmental factors, and infections.
When we know the markers to look for and understand the pathway to disease, we can work with people to address the specific cause(s) of inflammation and start turning back the clock.
Addressing Chronic Infections
Effective treatment requires a holistic view of a person’s immune system, nutritional deficiencies, sleep, stress, toxin exposure, and more, to support their body so it can begin clearing away some of these chronic infections.
On the one hand, treatment of chronic infections can get quite complicated, requiring advanced testing to identify the specific disease path. On the other hand, the treatment isn’t really complicated; the basic goal is to improve your immune system by getting the right amount of nutrition and fatty acids so that your body can stop over-responding to most infections.
My first advice to treat and prevent chronic infections is to: Eat real food, Manage your stress, and Get adequate sleep.

-
Eat Real Food
Remember that leaky gut was one of the common preconditions of both autoimmune and autoinflammatory diseases? Eating real food has a huge impact on your gut health. Looking for help to “eat real food?” Check out my free course: Real Food Diaries
-
Manage Your Stress
In the West, we have serious issues with stress and mental health problems leading to high cortisol and over-activation of the immune system, resulting in immune dysregulation.
-
Get Adequate Sleep
Sleep is critical to healing and resetting the immune system. Without good quality sleep, the body will not be able to recover adequately.
I refer to gut, stress, and sleep as The Triangle of Health, and I’ve used this threefold approach to develop multiple resources. These foundational lifestyle factors alone have a massive impact on chronic infections.
Adding things like mushroom extracts, leaf extracts, curcumin, probiotics, and immunoglobulins like IgG colostrum can also help your body appropriately control chronic infections. Certain interventions like low-dose naltrexone, peptides, treating sleep apnea, and removing mold from the environment can provide substantial improvement in helping the immune system not respond to the trillions of bacteria and untold numbers of yeast and viruses in their system.
Speaking of mold…
Addressing Mold
Obviously, the best solution to mold issues in a home or building is to remove the mold or remove yourself from the problematic environment. However, there are a few basic interventions that can have a major impact on your risk of CIRS or lower-grade chronic health issues; specifically: filter your air and increase your fiber intake.
-
Filter Your Air
Using a HEPA filter can reduce your exposure to these harmful substances in the air.
-
Increase Your Fiber Intake
Fiber in your diet can help your body to naturally bind and remove toxins.
The lack of fiber in the typical American diet has exacerbated mold-related illnesses. Primitive cultures typically would consume up to 100 grams of fiber a day. Today, the typical American consumes only 8 – 9 grams of fiber a day and the USDA only recommends 15 grams a day. Natural fiber is the key binder for many of these toxins. You can ncrease your fiber intake by using plant foods like flax, chia seeds, sunchokes, yams, or other root vegetables just to name a few.
Conclusion
I hope this article helps you understand how our perception of disease is changing and why our healthcare system needs to change with it.
We must pivot how we look at disease, and we really do need individualized health care. The current model of looking at symptoms and doling out treatments is inadequate. To address this changing landscape of chronic health illnesses, we need an army of well-trained practitioners, who are lifelong learners of the art and science of medicine, and who have a healthy respect for the complexity of health and illness.

Don’t Miss Out
Sign up for our newsletter and be the first to know when Dr. Hartman posts a new article.