Prevent Heart Disease with Food
Proactive Prevention for Our Deadliest Disease

Aaron Hartman MD
May 14, 2024
Subscribe
Never miss out on new content from Dr. Hartman.
Over the last several years, we seem to have lost sight of the most common killer in our country.



Heart disease, also known as cardiovascular disease, accounts for almost 660,000 deaths in America every year. Heart disease has been the number one killer in our nation for over 50 years. Unfortunately, heart attacks and heart disease still catch us off guard. We call it a “silent” killer. Why?
Consider these two statistics:
- Heart disease is missed by our current screening methods in over 50% of affected patients.
- While there are currently 395 known risk factors for heart disease, our current medical system screens for only five (diabetes, blood pressure, cholesterol, obesity, and smoking).
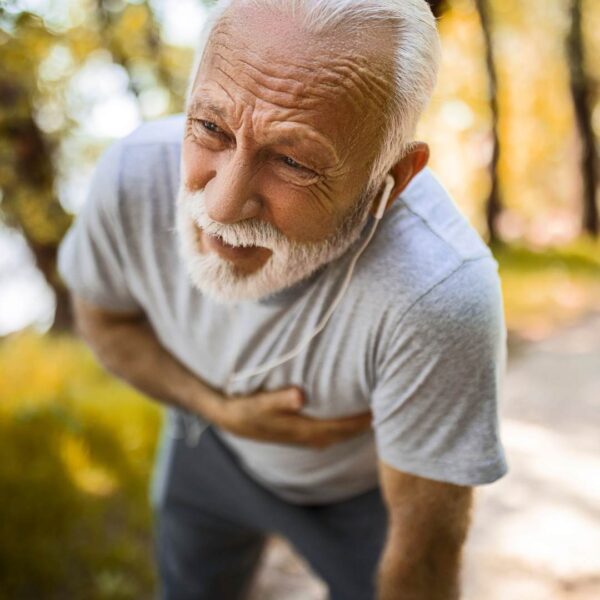
Our Present Approach to Heart Disease is a Problem, but the Horizon is Hopeful!
Let’s dig a little deeper into why I said that cardiovascular disease is still a “silent” killer:
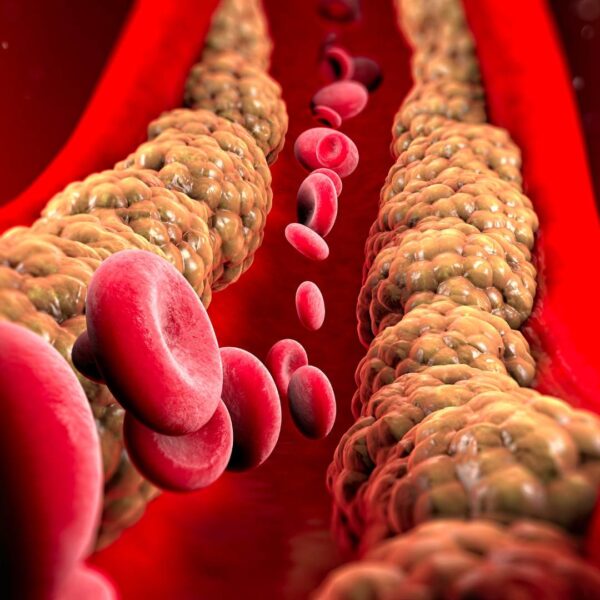
- 60% of those who have a heart attack have less than a 50% blockage of their artery.
- 50% of those who present to the emergency room with their very first heart attack have normal cholesterol levels.
- 62% of men who have a heart attack have no previous diagnosis of heart disease.
- 46% of women who have a heart attack have no previously recognized heart disease symptoms at all.
As you can see, our current methods of screening for the number one killer in our country is woefully inadequate.
So how can you be proactive in preventing the number one cause of death?
Some Good News
There is a lot of new research around cardiovascular disease. In fact, a new field of study sometimes referred to as metabolic cardiology, cardiometabolic health, or translational cardiovascular medicine, examines the complex data surrounding an individual’s personal risk for heart disease. Currently, cardiometabolic medicine is only practiced at a few centers around the country, including the Vanderbilt Hypertension Clinic with Dr. Mark Houston, who notably started the very first cardiometabolic fellowship in the country.
Screening for Heart Disease
Let’s briefly examine the traditional markers for heart disease to see why these screening tools are inadequate for preventing this silent killer. Then, I’ll address some more advanced screening options that paint a better picture of a person’s real risk for heart disease.
Basic Screening

Blood Pressure
What’s normal blood pressure? You’ll hear 140 over 90 is normal. But what if I told you a blood pressure higher than 110 over 70 was associated with an increased risk for heart disease? Simply addressing an elevated blood pressure with medication and ignoring the root cause of the problem does not effectively promote better cardiovascular health.
Cholesterol
Traditional recommendations set normal total cholesterol as less than 200 and LDL as less than 100 or 120. But current data shows that a cholesterol LDL of over 60 starts to lay down plaque in your arteries.
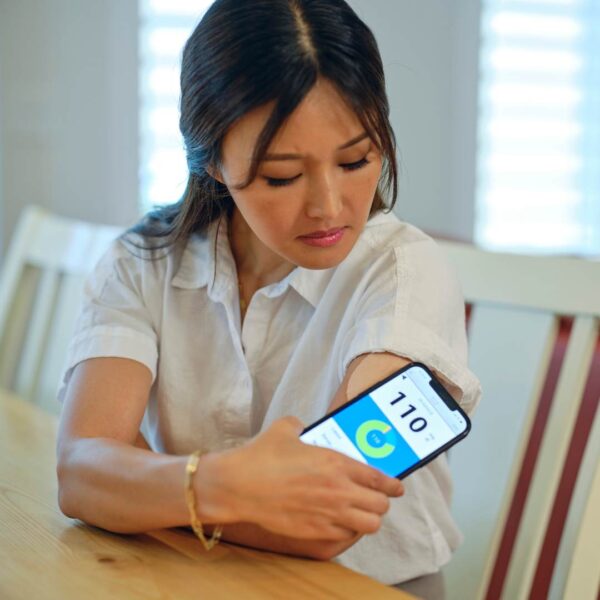
Blood Sugar
What is a normal fasting sugar level? We hear that normal fasting blood sugar is 100 or less. Actually, a normal fasting blood sugar, below which there’s no increased risk of heart disease is 75. For every one point, the fasting blood sugar is above 75, there’s a 1% increased risk for heart disease. So a fasting sugar of 100 has a 25% increased risk for heart disease. And you’re not even considered by the American Endocrinological Society as being close to being diabetic in these ranges.
Smoking
Obviously, smoking is terrible for your health. I implore you not to smoke. For the purposes of this article, however, I will only note that while smoking DOES contribute significantly to heart disease, the absence of smoking DOES NOT, by itself, prevent heart disease.
Obesity
Obesity is another oversimplified metric that fails to account for the necessary data. Over the last 20 years, we’ve learned that “visceral fat,” the accumulation of fat in and around the internal organs (including your liver and heart), is much more damaging than “subcutaneous fat,” the fat under your skin. This is where we get the term “skinny fat” — people who are not obese but have fat accumulated around their organs.
As you can see, our current screening methods underestimate our risk of heart disease. Why?
Why is Current Screening for Heart Disease Inadequate?
When we use more advanced numbers, we see that
- About half of Americans have high blood pressure issues.
- 50% of Americans are either diabetic or pre-diabetic, and 80% have some level of insulin resistance.
That’s a lot of people who should be flagged for conversations and interventions. Our medical system simply can’t deal with these kinds of numbers. Screening methods need to be feasible in a primary care office where physicians have 10–12 minutes to talk to patients. So “normal” numbers are set too high and we’re surprised when “normal” adults unexpectedly suffer from heart attacks.
Screening methods need to be feasible in a primary care office where physicians have 10–12 minutes to talk to patients. So “normal” numbers are set too high and we’re surprised when “normal” adults unexpectedly suffer from heart attacks.
That’s the bad news … but there is still hope.
Individualized, functional medicine uses a different model of care that affords more time, and attention. When data points toward earlier warning signs, functional doctors do not turn a blind eye to risk factors that take time to unpack and unwind. A functional medicine physician can use a more comprehensive approach to evaluate your risk factors and not just use a simple template when assessing your risk.
Advanced Screening for Heart Disease
Advanced screening includes stricter metrics for blood pressure, blood sugar, cholesterol, and visceral fat, as well as screening for underlying root causes like: inflammation, immune dysregulation, and oxidative stress.
Inflammation
We’re now seeing a correlation between infection, inflammation, and heart disease. Because inflammation is a risk factor for cardiovascular disease, there are advanced tests we can use to assess inflammation and therefore get a better understanding of the risk for cardiovascular disease. High-sensitivity C-reactive protein (hsCRP) is a measure of inflammation in your arteries related to liver function. We also might look at homocysteine, which is a metabolic measurement for inflammation. High homocysteine levels can also be associated with vitamin deficiencies.
Ultimately, inflammation is a dysregulation of the immune response. There are further tests to assess immune dysregulation. We might use tests like interleukin-1 (IL-1), interleukin-6 (IL-6), tumor necrosis factor-alpha (TNF alpha), interferon-beta, and others that measure cytokines related to the immune response.
Cholesterol
We might look at cholesterol at a more granular level, by breaking it down into the more important risk factors like LDL particles and apolipoprotein B. There are over 20 different breakdown products in cholesterol that can be used to assess risk factors through the Cleveland HeartLab. This level of testing comes at a high financial price. These cost about $200 and insurance does not pay for them, so they are not often considered. When other risk-factors prompt a need for more data, however, it is important to know this screening is available.
Calcium Buildup
Then there is advanced testing that measures calcium buildup, like a coronary artery CT, which measures the calcium buildup in the arteries in the heart, a marker of late-stage heart disease. It is possible to have a stress test that’s normal, a catheterization that’s normal, yet still have a high calcium score. I see this all the time.
Other Advanced Screening Options
- Carotid ultrasounds measure the artery wall thickness and can actually pick up changes before calcium is laid down.
- EndoPAT assesses endothelial function (endothelial cells main type of cell found in the inside lining of blood vessels, lymph vessels, and the heart).
- Computerized Arterial Pulse Wave Analyzer (CAPWA) is another advanced screening option.
All these need to be done under the careful guidance of a metabolically-trained physician, typically through either the tutelage of Dr. Houston through the Institute for Functional Medicine (IFM), the American Academy of Anti-Aging Medicine (A4M), or some similar organization.
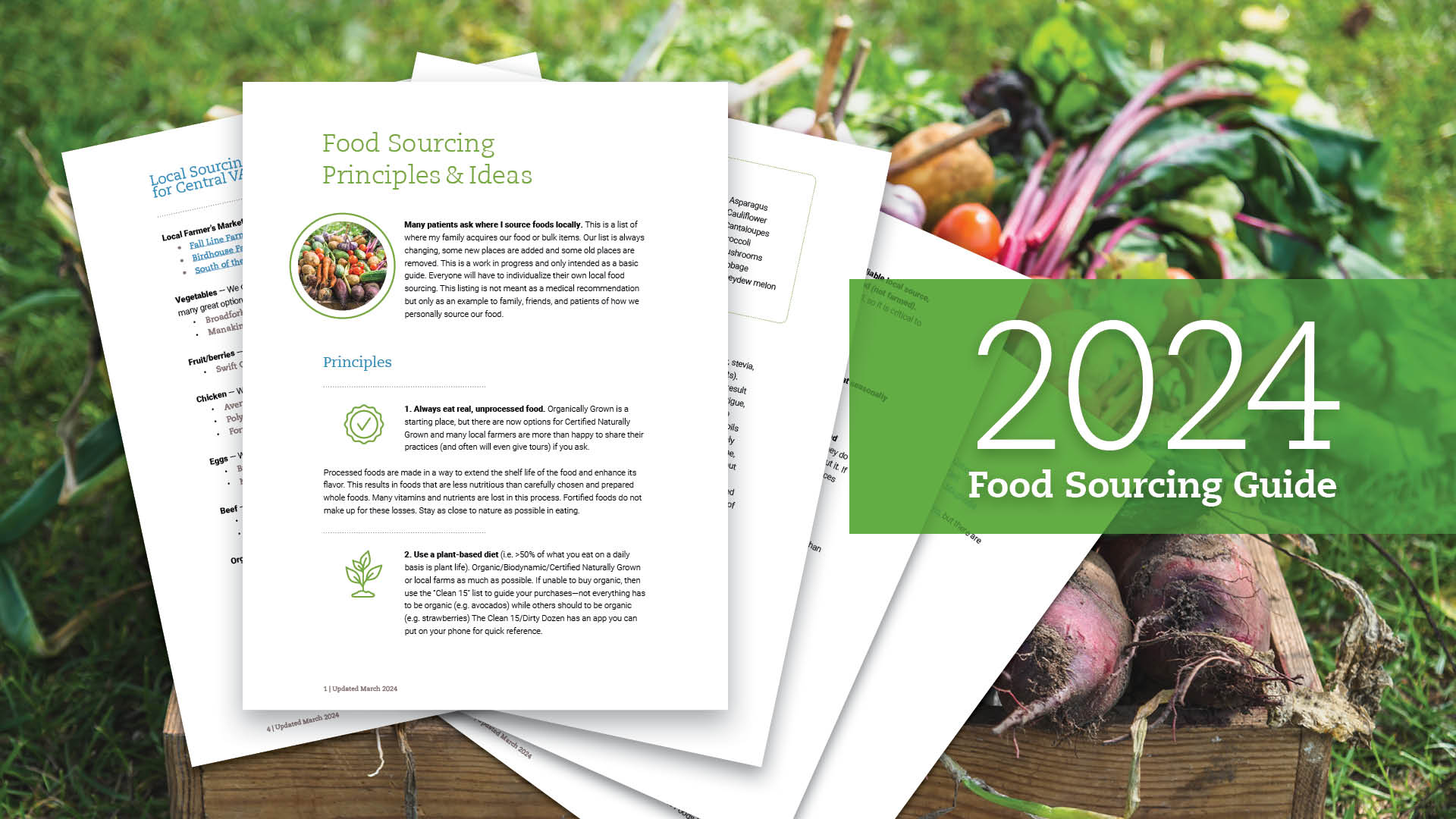
Food Is Medicine
The foundations of a healthy lifestyle include diet, exercise, adequate sleep, stress reduction, and relationships. Heart health is no exception.
As always, I encourage you to focus on The Triangle of Health: Gut • Stress • Sleep.
In this article, I will focus primarily on food as medicine, but I urge you not to forget that stress kills and sleep heals. Sleep and stress management are lifestyle medicine. Preventing heart disease will always require that you balance the Triangle of Health.
But let’s turn to the powerful role of food in preventing heart disease.
The food you eat can be either the safest and most powerful form of medicine or the slowest form of poison.
—Anne Wigmore
Diet is always the key part of any health protocol. 90% of your immune system is in your GI tract. What you eat becomes the building blocks your body uses to build and heal. Food also communicates important messages to the body and modulates your metabolism. Conversely, our diet is also one of the major sources of toxins and inflammation in the body.
Could diet alone have a truly significant impact on the number one killer in our country? And if so, what would such a diet look like?
To answer these important questions, let’s briefly survey some of the landmark studies that inform how we understand the role of food in causing or preventing heart disease.
Research in Diet & Heart Disease
The Framingham Heart Study
Why Don’t We Hear about the Effects of Diet?
We’ll start with one of the biggest studies to date that people talk about, which is the Framingham Heart Study. This study, based in the UK, evaluated over 10,000 patients for medications and other heart disease treatments, but the dietary aspect of this study is often overlooked. The Framingham Study showed that nondescript “CV-lowering or lipid-lowering diets” decreased total cholesterol, triglycerides, and increased HDL. Unfortunately, in this pivotal trial, detailed specifics on diet weren’t studied, hence more research was needed.
The Seven Countries Study
Overlooking the Quality of Dietary Fat
The Seven Countries Study was an international study that looked at lifestyle and diet. A high-fat diet was shown to increase the prevalence of heart disease. This is where we get the idea that fat in the diet causes heart disease. But the study didn’t specify what kind of fat was a healthy fat or an unhealthy fat, which would have been a great question. We now know that healthy fats can actually contribute to heart health, which I’ll discuss further below.
The Pritikin Diet
Did Diet or Exercise Improve Cholesterol?
The Pritikin Diet showed the ability to improve cholesterol. This diet is a low-fat diet, consisting of only 10% of calories from fat, and includes primarily vegetables, grains, and fruits, and is also combined with exercise. We’re starting to see some conflicting data based on how these trials were designed.
The Ornish Diet
Is it the Diet, Exercise, Stress-Reduction, or Smoking Cessation That Causes the Benefits?
Dean Ornish has been well-known for his vegetarian-style, low-fat diet (again 10% of total calories). The Ornish diet includes lots of complex carbs, low refined (processed) carbs, and low dietary cholesterol and is combined with exercise, stress reduction, and smoking cessation. This diet showed a reduction in all-cause mortality, total cholesterol, and showed many other benefits. At year five, there was a reduction in calcium build-up in the heart, heart attacks, strokes, and overall deaths.
These findings popularized vegan-style diets, while his lifestyle change and stress reduction aspects were largely overlooked. These are some of the reasons I like to read the actual research to find out what was really studied, not what secondary sources say about them.
The Portfolio Diet
Studying the Numbers Instead of Actual Health Outcomes
The Portfolio diet study was another big trial that included a vegetarian-type diet with soluble fiber, nuts, soy protein, and plant sterols to see how they affected cholesterol numbers. The interesting part about this is that actual outcomes like death and heart attacks weren’t the focus, but they did show that total LDL cholesterol fell 29.6% and triglycerides fell almost 10%. In comparison, the group that received cholesterol-lowering medication had a 33% reduction in total cholesterol. The difference between the dietary intervention and the medication intervention was not statistically different.
The Lyon Diet Heart Study
A Study Using Healthy Fats
This was the first single-blind prevention trial of its kind. Over four years it looked at the endpoints of heart attack and cardiovascular disease. The primary outcome evaluated was whether heart attack victims lived or died after the attack. These are important outcome data points.
The Lyon diet included 30% of calories from fat. You heard me right, 1/3 of the diet was fat, but it was healthy fat — about 12% were monounsaturated fatty acids like olive oil and it was enriched with alpha-linolenic acid (ALA), which is the primary omega-3 from seeds. Flax seeds are actually the most abundant source of alpha-linolenic acid. In this study, they found cardiovascular disease prevention in 20 – 30% of all major events.
The PREDIMED Study
Lowering Inflammation and Heart Disease with Olive Oil
The PREDIMED Study was a three-month randomized trial based in Spain. The study showed that consuming about a liter of extra virgin olive oil per week lowered all the inflammatory markers for heart disease. You read that correctly; healthy fat lowered cardiovascular inflammation. In this study, hsCRP, interleukin 6 (IL-6), ICAM-1 (Intercellular Adhesion Molecule 1), VCAM-1 (vascular cell adhesion molecule one) all were reduced. All these were lowered with a simple intervention of extra virgin olive oil. When you dive into the deep science, the inflammation (measured by these markers) is what actually causes heart disease, not the cholesterol itself.
So what does that mean? This means food really is medicine, especially for your heart. What matters most in evaluating these studies is a heart attack, stroke, and death. Ultimately we should be focusing on outcomes, not numbers like cholesterol. That’s the most important aspect of evaluating research, trials, and treatment.
Ultimately, we don’t treat statistics, we treat patients; the most important thing to a patient is the outcome.
Nutritional Interventions
Foods & Supplements that Can Reduce Your Risk of Heart Disease
Building on the foundation of a quality diet and healthy lifestyle, scientifically-proven nutrition and nutraceuticals can have a powerful effect on cardiovascular health and healing.
We can use food as medicine and nutrients like drugs.
Ideally, you should work with a practitioner who understands how to use lab testing to determine which nutrients would be most helpful to you, how to source them, and how to use them appropriately. Using nutraceuticals can actually be more complicated than medications and drugs as there are more options, more interactions, and more data with nutrition than medications. This is a striking statement to make since our primary treatment currently is medications, not nutrition.
The most important nutrients for reducing your risk for cardiovascular disease are:
- Niacin
- Red rice yeast
- Plant sterols (phytosterols)
- Green tea (EGCG)
- Omega-3s (especially Alpha-linolenic acid or ALA)
- Flax seeds
- Monounsaturated fatty acids (MUFAs)

Niacin (Vitamin B3)
Niacin is an important nutrient in cardiovascular disease prevention for its role in various benefits. It has been shown to lower total cholesterol, lower triglycerides, and reduce LDL particle numbers.
A typical dose is between 500 milligrams up to four grams daily. Interestingly, lower doses of vitamin B3 have a more profound effect on elevating HDL, which is your healthy cholesterol. Higher doses have a more profound effect on lowering LDL. So the dose should depend on whether your goal is to increase HDL or lower LDL.
Mass trials such as the Coronary Drug Project (CDP), the HDL-Atherosclerosis Treatment Study (HATS), the ARBITER 2 trial, the Oxford Niaspan Study, and the Familial Atherosclerosis Treatment Study (FATS), have shown a reduction in heart events and coronary plaque build-up with niacin. There is even a prescription version called Niaspan, so the FDA even acknowledges that niacin is an effective treatment and preventative for cardiovascular disease.

Red Rice Yeast
Red rice yeast is the next heavy hitter. A fermented rice product, red rice yeast contains over 13 natural statin-like properties, as well as amino acids, flavonoids, trace elements sterols, monounsaturated fatty acids, and a whole host of anti-inflammatory molecules.
Combined with berberine and other plant sterols, red rice yeast has been shown to lower cholesterol anywhere from 20 – 30%. In a Chinese study of over 4,000 patients over almost five years, red rice yeast lowered the risk of heart disease death by 30%!
One caveat with red rice yeast is that, if it’s not packaged appropriately, it can become contaminated with mold toxins, since it is a fermented product. If you have used red rice yeast in the past and have experienced muscle aches and pains, it’s likely that it was caused by contamination of a mold-related mycotoxin and not from the red rice yeast itself. This is one of the many reasons we recommend high-quality nutrient products and not some of the cheaper over-the-counter brands.

Plant Sterols (Phytosterols)
Plant sterols are typically sourced from maritime pine trees. Some lesser-quality products come from soybeans; definitely avoid those. Plant sterols work by decreasing the reabsorption of cholesterol in the GI tract, and they also lower inflammation. They reduce hs-CRP, interleukin 6, TNF alpha, and fibrinogen levels. Fibrinogen is especially associated with tiny blood clots (microclots) and small arterial disease.
In combination with berberine and niacin, the phytosterols can support cardiovascular health and healing. Studies have shown a total cholesterol reduction from 8 – 10% and an LDL reduction from 6 – 15%. A typical dose is between 500 – 1000 mg. Higher doses of this nutrient don’t necessarily give a better result.
One side note is that, because plant sterols do affect lipid metabolism, they can potentially reduce levels of vitamins D, E, K, and alpha-carotene. Either supplementing with these or testing these nutrients to make sure they are not lowered is appropriate.

Green Tea (EGCG)
EGCG is another great nutraceutical for lowering cholesterol. It’s been shown to reduce oxidized LDL, upregulate LDL receptors, and lower inflammation. The pharmaceutical dosing is 4 – 6 cups of green tea a day, or 500 – 1000 mg daily of EGCG. This is such a simple add-on with a slew of benefits, including improving insulin sensitivity and improving hormone detoxification just to name two in addition to the cholesterol-lowering effects.

Omega-3 Fatty Acids
Omega-3s are a powerful nutraceutical with so many positive effects on health, including cardiovascular health. They have become one of the top recommendations for heart attack and stroke reduction as well as for lowering cholesterol and triglycerides. Data has shown that omega-3 fatty acids can lower the risk for coronary events by about 20%, strokes by about 22 – 25%, and sudden cardiac death by up to 45 – 50%.
Omega-3s also have anti-inflammatory, blood-thinning, and cholesterol-lowering properties. They are one of the few nutrients that reduce a molecule called Lp-LPA2, which is a very inflammatory molecule associated with acute stroke and heart attack. Typical doses range from 1000 – 3000 mg.
Be sure to balance your omega-3s with GLA (Gamma-linolenic acid) as well as vitamin E, since excessive amounts of fish oil can sometimes induce insulin resistance and make your sugars go up slightly.

Flax Seeds
Flax seeds are another of my favorites. Note that the effects of flax seeds do not apply to flax oil. Flax seeds are a much more comprehensive and traditional type of pharmaceutical. The fiber, lignans, phytoestrogens, and plant sterols have a multitude of effects that the oil by itself does not provide. Flax seeds promote anti-inflammatory effects, lower hs-CRP, reduce triglycerides, increase HDL (good cholesterol), and improve insulin sensitivity. For women, flax seeds help modulate hormones and lower the risk for both heart disease and breast cancer by about 25%.

Monounsaturated Fatty Acids (MUFAs)
Finally, I’d like to talk about monounsaturated fatty acids (MUFAs), the best source of which is extra virgin olive oil. Olive oil has been shown to lower total cholesterol by 10 – 15%, LDL and triglycerides by 10%, and increase HDL by about 5%. Olive oil lowers oxidized LDL, one of the major causes of artery disease, better than almost any other substance. It’s also an anti-inflammatory, helps modulate the bacteria in your gut (your microbiome), and helps with weight maintenance.
Typical dosing is between 30 – 40 grams a day or three to four tablespoons if you’re using it pharmacologically. According to some of the research from Dr. Gundry, author of The Plant Paradox, up to nine tablespoons of olive oil a day will give you a strong cardiovascular-protective effect. I find that four tablespoons per day are a dose that most people are more likely to stick to.
There are many other nutraceuticals or nutritional substances that have drug-like strengths that we haven’t talked about. We have not talked about tocotrienols, pantethine, resveratrol, garlic, curcumin, vitamin C, citrus bergamot, lycopene, flavonoids, or berberine.
The point here is that there are many simple foods and food concentrates that have medicinal-type strengths and usages. It’s important to understand that all these things should be an add-on to the foundations of health: diet, lifestyle, exercise, sleep, and stress reduction. This is a strong combination that can have a powerful impact on your cardiovascular health and longevity.
Summary
The extensive research and insights presented underscore the profound impact that diet and nutraceuticals can have on cardiovascular health.
By embracing a holistic approach that includes a diet rich in omega-3 fatty acids, extra virgin olive oil, and incorporating nutraceuticals such as niacin, red rice yeast, and green tea, you can significantly reduce your risk of heart disease. In fact, when you combine the data from the studies above with the nutraceuticals listed, we can induce an LDL reduction of up to 50% in patients with significantly elevated LDL. This is superior to any drug on the market.
I encourage you to take these insights to heart and proactively incorporate these healthful practices into your daily life. By doing so, you not only enhance your heart health but also improve your overall well-being, offering a promising way to lead a longer, healthier life.